 BUDDI API Marketplace
BUDDI API Marketplace Launching
for all your healthcare API needs
Our Deep Learning Platform
Solutions
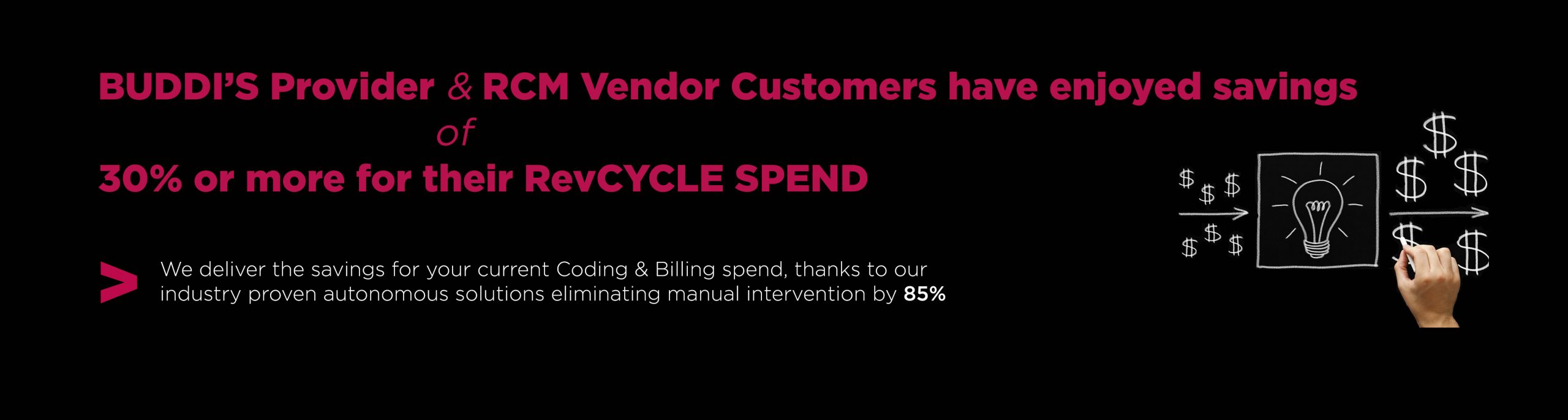
BUDDI.AI streamlines the most important clinical and revenue cycle functions.
CODING.AI
Powered by industry-leading deep learning algorithms, CODING.AI is the most accurate medical coding automation platform on the market. CODING.AI automates the majority of provider coding volumes, resulting in more accurate claims, fewer denials, and higher reimbursements – guaranteed by industry-leading SLAs.
BILLING.AI
BILLING.AI automates the end-to-end medical billing process, including charge entry, eligibility verification, denial prediction, and prevention, claim preparation, claim submission, adjudication, response, and A/R redirection. Also included is our comprehensive analytics dashboard, which includes 140+ detailed reports and proactively identifies opportunities to maximize revenues.
CODECOMPLIANCE.AI
CODECOMPLIANCE.AI leverages optical character recognition and deep learning models to examine generated medical codes and increase compliance with CMS guidelines. Additionally, it extracts the medical record data from various formats and automatically generates a comprehensive audit report (per physician) with detailed feedback to drive performance improvement.
PRIORAUTH.AI
PRIORAUTH.AI automates clinical procedure identification from unstructured medical records and cross-references these procedures against payer prior authorization lists. Imagine freeing up hundreds, if not thousands of additional man-hours by automating prior authorization identification and submission.
REGISTRATION.AI
REGISTRATION.AI simplifies the front-end patient intake process for providers. Capture demographic information electronically, verify patient insurance eligibility, co-pay, co-insurance, and deductibles across 3,000+ payers in real-time, and allow patients to e-sign pertinent documents prior to their scheduled appointments. REGISTRATION.AI enables providers to deliver a seamless patient experience.
PRACTICE.AI
Practice.AI automates end-to-end revenue cycle processes using NLP, Grpah, Logic based rules. The platform automates medical codes ( CPT, ICD 10, Modifiers, MIPS, G-Codes, Z-Codes ), bill ready charges, eligibility verifications, denial prediction and prevention, claim preparation, claim submission, claim reappeals, A/R workflow queue optimization, payer contract onboarding, payer contract analysis, underpayment analysis, EOB/ERA root cause analysis for line item wise denials.
CDI.AI
CDI.AI evaluates physician notes in real-time and provides swift feedback on areas of improvement. This decreases the administrative burden on physicians and improves the quality of patient care. As providers transition from fee for service to value-based care, implementing CDI.AI is a proactive step toward enabling quality care and a healthy revenue cycle.
MEASURES.AI
MEASURES.AI processes the clinical record through a deep-learning engine and validates it against the four MIPS performance categories: quality, cost, improvement activities, and promoting interoperability. MEASURES.AI gives providers and administrators real-time insight into their composite score, the ability to identify and correct care gaps and report measures directly to CMS.
ClINICAL.AI
ClINICAL.AI leverages our proprietary 'Medical Language Processing' technology to extract important clinical information from health records with over 95% accuracy, powering an array of use cases including, but not limited to: diagnostic error prevention, clinical decision support, clinical trial patient matching, pharmacovigilance, and medical image analysis.
CLAIMS.AI
CLAIMS.AI analyzes historical denials and approvals, as well as EOBs, medical codes, CARC/RAC codes, payment patterns, and other payer behavior to proactively identify errors before claim submission, decreasing odds of denial. Clients who have deployed Claims.Ai report a 40% average reduction of denials within 12 months of launch.
CODING.AI
Powered by industry-leading deep learning algorithms, CODING.AI is the most accurate medical coding automation platform on the market. CODING.AI automates the majority of provider coding volumes, resulting in more accurate claims, fewer denials, and higher reimbursements – guaranteed by industry-leading SLAs.
PRIORAUTH.AI
PRIORAUTH.AI automates clinical procedure identification from unstructured medical records and cross-references these procedures against payer prior authorization lists. Imagine freeing up hundreds, if not thousands of additional man-hours by automating prior authorization identification and submission.
MEASURES.AI
MEASURES.AI processes the clinical record through a deep-learning engine and validates it against the four MIPS performance categories: quality, cost, improvement activities, and promoting interoperability. MEASURES.AI gives providers and administrators real-time insight into their composite score, the ability to identify and correct care gaps and report measures directly to CMS.
CLINICAL.AI
CLINICAL.AI leverages our proprietary 'Medical Language Processing' technology to extract important clinical information from health records with over 95% accuracy, powering an array of use cases including, but not limited to: diagnostic error prevention, clinical decision support, clinical trial patient matching, pharmacovigilance, and medical image analysis.
CODING.AI
Powered by industry-leading deep learning algorithms, CODING.AI is the most accurate medical coding automation platform on the market. CODING.AI automates the majority of provider coding volumes, resulting in more accurate claims, fewer denials, and higher reimbursements – guaranteed by industry-leading SLAs.
CLINICAL.AI
CLINICAL.AI leverages our proprietary 'Medical Language Processing' technology to extract important clinical information from health records with over 95% accuracy, powering an array of use cases including, but not limited to: diagnostic error prevention, clinical decision support, clinical trial patient matching, pharmacovigilance, and medical image analysis.
Outcomes we drive
Don't let your fear of change prevent you from achieving breakthrough results.
We’re the only company in the industry that contractually guarantees accuracy and automation volumes.
Core Metrics
Partners

Microsoft
BUDDI.AI's HIPAA and SOC 2 compliant platform is deployed on Azure, Microsoft's industry-leading cloud platform.
Learn morePartners

Redox
Our partnership with Redox enables BUDDI.AI to seamlessly integrate with your existing EMR solution to facilitate secure, standardized health data exchange.
Learn morePartners

IIT Madras
BUDDI.AI has partnered closely with IIT Madras, the "MIT of India" to develop the most accurate, most robust deep learning algorithms for healthcare.
Learn moreIndustry Perspectives
AI and Revenue Cycle Management: Ushering in a New Era
Replacing computer-assisted coding (CAC) and robotic process automation (RPA) with an AI-powered automation platform will deliver greater accuracy, cut turnaround time, save significant dollars and drastically improve operational efficiency.
Download EbookTechnology
We know that AI seems complicated
Perhaps you tried to build it in-house and failed (this happens 87% of the time, according to VentureBeat), or you’ve avoided it altogether. The good news is that we’ve done the heavy lifting for you.
Learn moreCompany
Expertise across the entire healthcare value chain
Our experts have decades of experience in AI and healthcare and have trained our algorithms using 40 million+ medical records across all specialties.
Learn moreGet Started Today
Schedule a demo to learn more about our portfolio of AI-powered applications for healthcare.
Request Demo