The future of revenue cycle automation is here
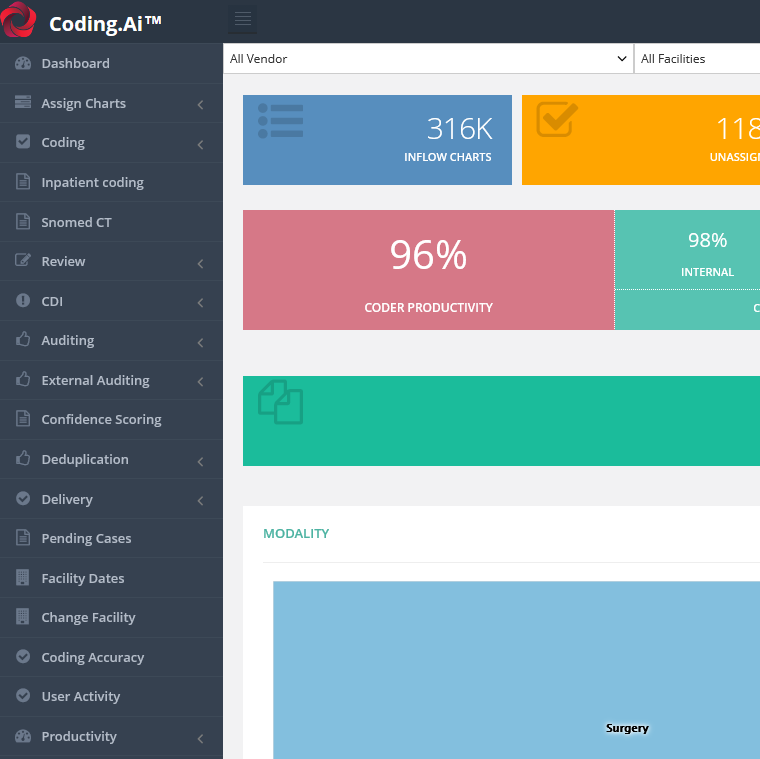
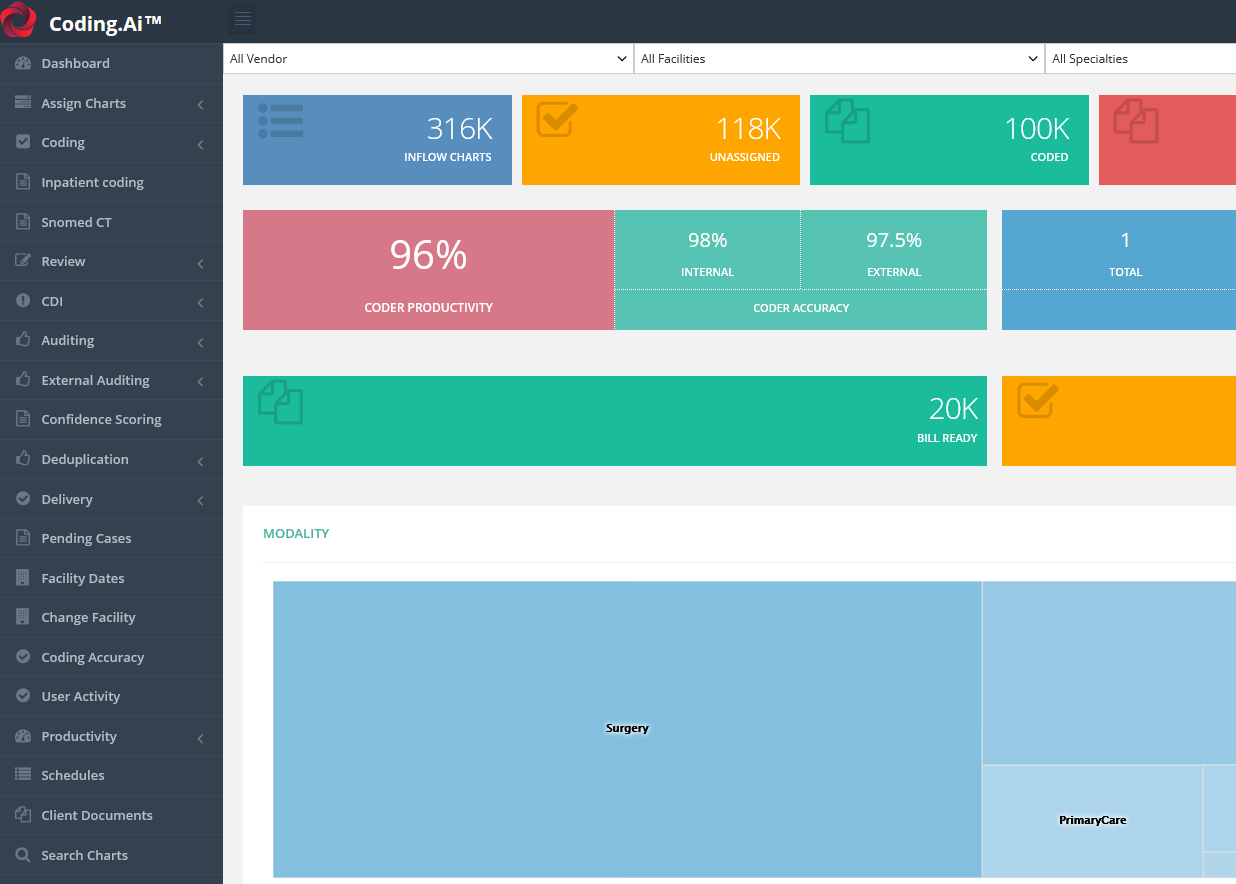
70% automation of bill ready codes and claims with 95+ accuracy
Outcomes
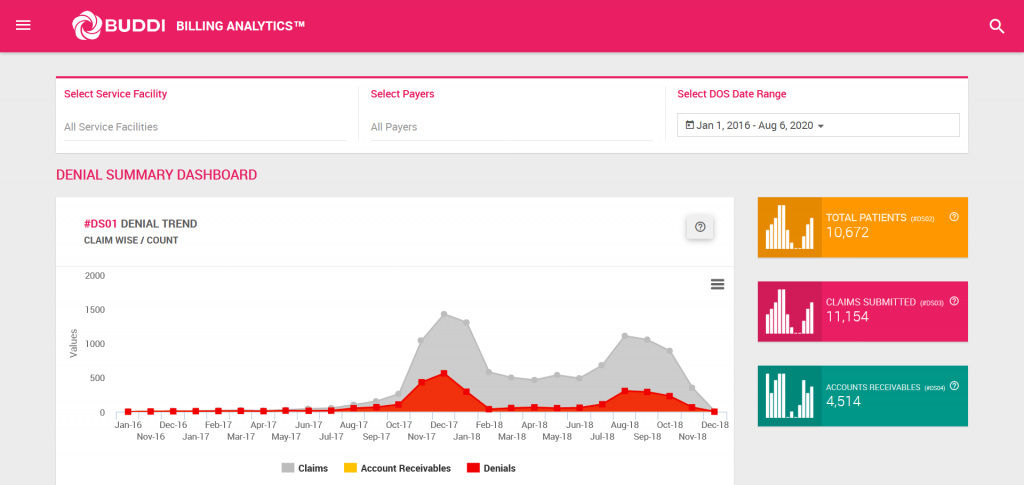
Automate claims submission, identify key trends, and improve your bottom line
BILLING.AI automates the end-to-end claims submission process while learning from historical payer denials and approvals to reduce claim denials by 40% within 12 months of go-live. BILLING.AI also delivers a comprehensive analytics dashboard with 140+ detailed reports salient to a provider's financial operations.
Automate billing workflows
Manual processes plague the prevailing medical billing workflow, causing providers to leave significant dollars on the table. BILLING.AI automates the end-to-end medical billing process, including charge entry, eligibility verification, denial prediction and prevention, claim preparation, claim submission, adjudication, response, and A/R redirection.
Identify key trends
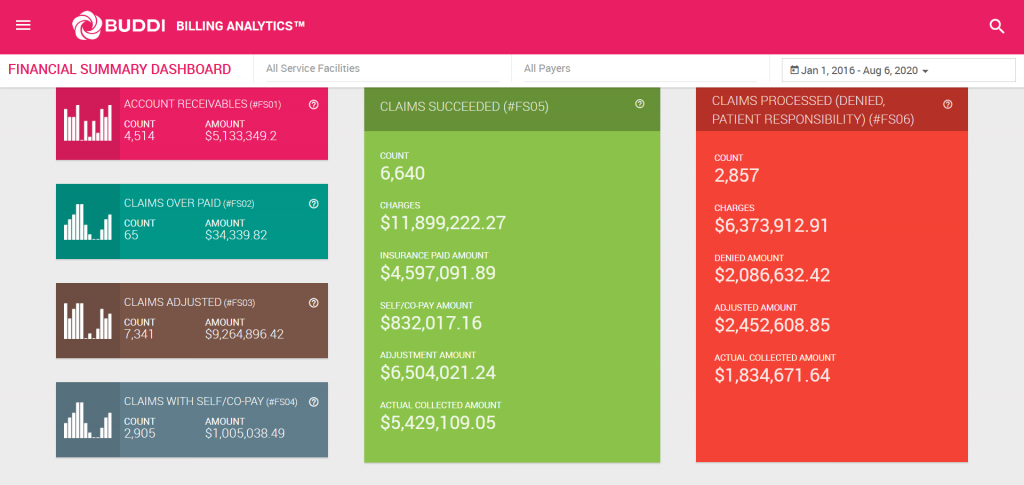
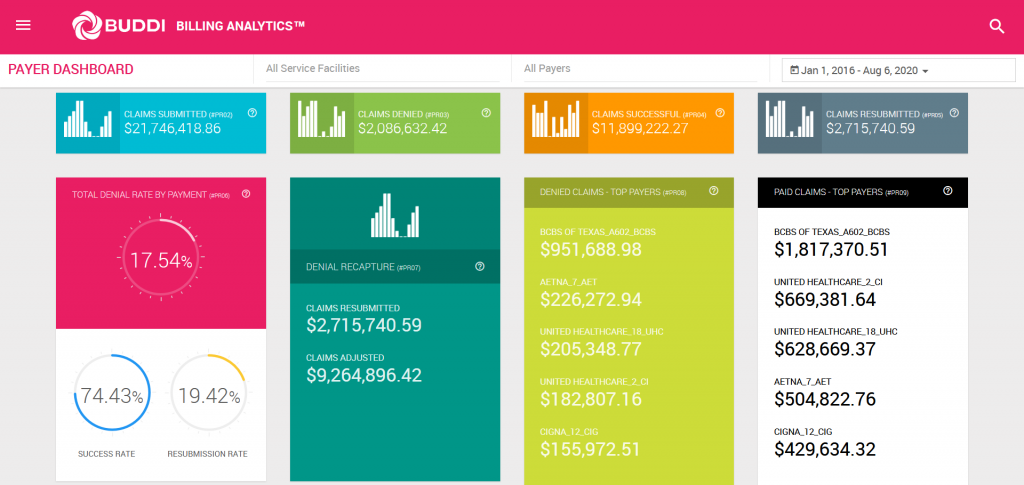
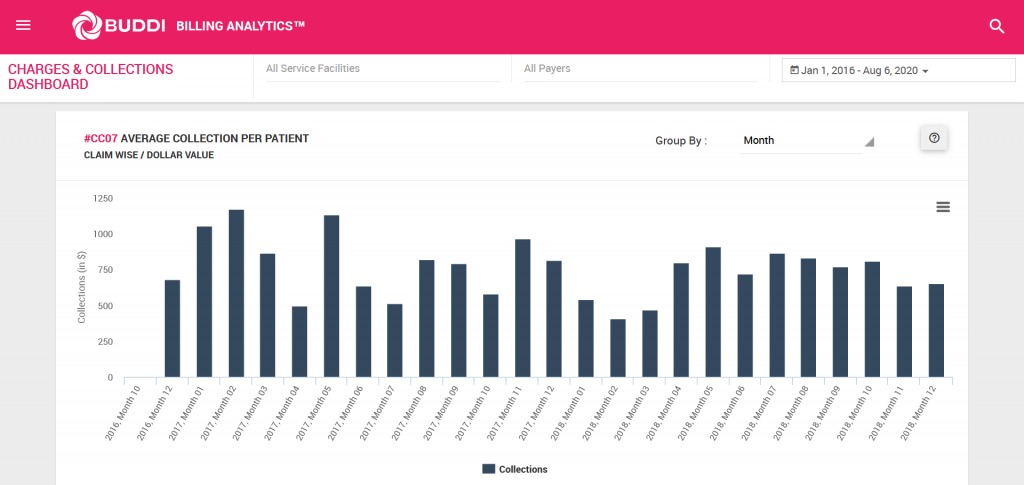
Our best-in-class billing analytics module includes 140+ detailed reports that track an array of details salient to a provider’s financial operations. BILLING.AI automatically identifies and summarizes key trends so that you can take action.
Improve your bottom line
Prevent revenue leakage, reduce costly billing mistakes, and streamline the currently cumbersome claims submission process by automating your end-to-end billing workflow. Leverage BILLING.AI to reduce the lead time to get reimbursed for services rendered. BILLING.AI helps providers get paid more, quicker.
BILLING.Ai
Features
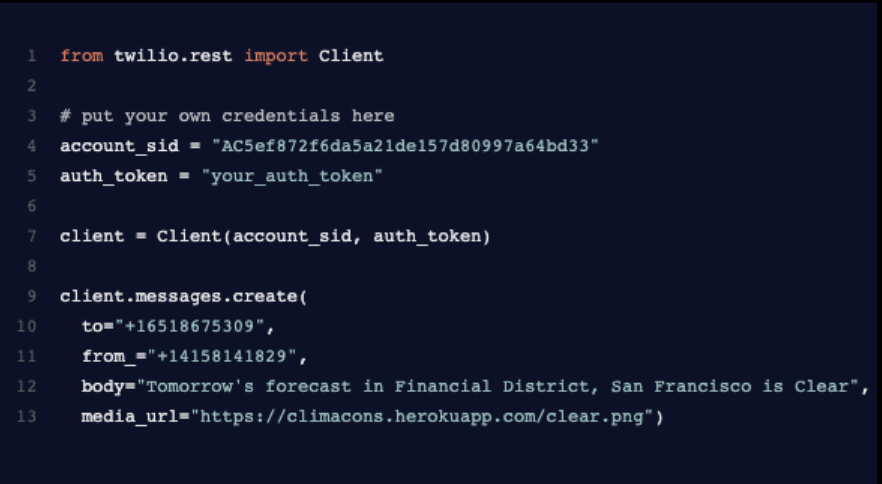
- Extensive interface capabilities which enable the import and normalization of patient data into the billing system.
- File formats accepted include HL7, JSON, and XML.
- Automated data error classification into various buckets to audit for discrepancies. Sample buckets include missing demographic information, missing coding information, and/or missing insurance information.
- Charge entry automation and specialty-based classification of charge entry.
- Automated claim adjudication is carried out based on various factors including eligibility verification and coding validations.
- Eligibility verification includes validation of co-pay, co-insurance, procedure eligibility, place of service, specialty, and in/out of network eligibility.
- Coding validations include: gender-specific procedures, age-specific procedures, medical necessity, maximum units, procedure corresponding to DOS and POS, procedure modifier, CCI, add-on procedures, LCD and NCD, applicable diagnosis and sequencing, and NPI.
- Denial prediction: Adjudication outputs contribute to the prediction of the denial score on a scale of 1-10 (with 1 representing an unlikely denial, and 10 representing a near-certain denial).
- Automation of claim preparation in 837 format and submission to the clearinghouse and payers.
- Automated parsing of the 835-formatted response and automatic posting of payments to the respective claims in the billing system.
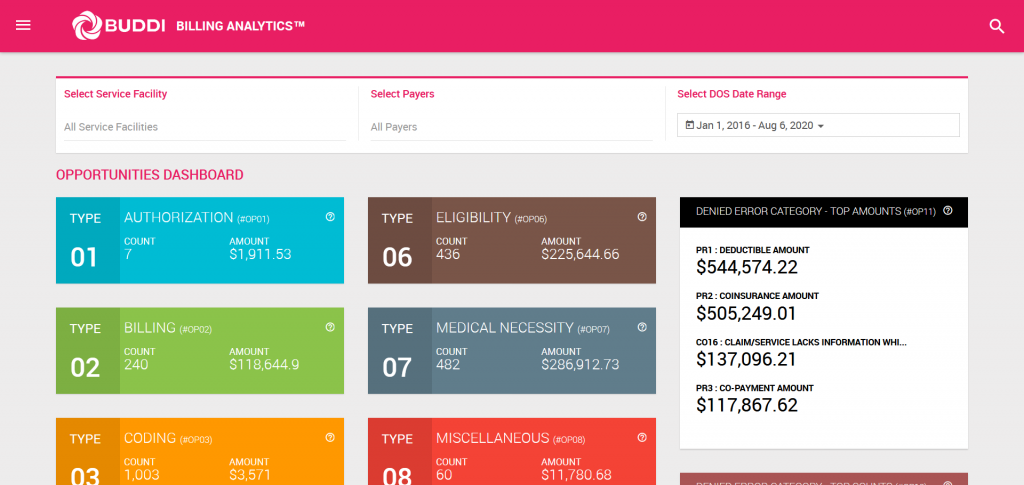
- Remark and remit codes from the 835 responses are analyzed and the claims are classified into denial-resolving opportunities.
- The following are the denial reduction opportunity buckets: authorization, billing, coding, contractual, duplicate, eligibility, medical necessity, miscellaneous, non-covered, and patient responsibility.
- Automated redirection of claims that are eligible for A/R to A/R management.
- Extensive billing analytics dashboard that provides real-time insights (140+ types) into claims data and identifies opportunities to reduce denials.
- Report types include financial summary dashboards, dashboard for claims in A/R, denial category and error category dashboards, statistics by payer and provider, highest dollar claim denials, high frequency denials, top denial reasons, top denials by payer, top denials by specialty, reclaim rate, claim-level denials, payment analysis, first-pass rate for claims, and claims aging summary.
Learn more about BILLING.AI
Schedule a demo today to see end-to-end billing automation in action.
Learn more